At Personify Health, we’re on a mission to redefine excellence in healthcare service delivery with a unique combination of high tech and human experiences. A recent infusion of top industry leaders and key investments is driving continued innovation and enhancement within our Third Party Administration (TPA) business, positioning us – and our clients – for success. Our relentless focus on operational excellence, member satisfaction, and claims precision is the cornerstone of this transformation, driving measurable improvements and future-ready capabilities.
Elevating Leadership Across TPA Operations
We are thrilled to welcome a powerhouse leadership team whose extensive expertise and visionary approach will spearhead our TPA growth and innovation:
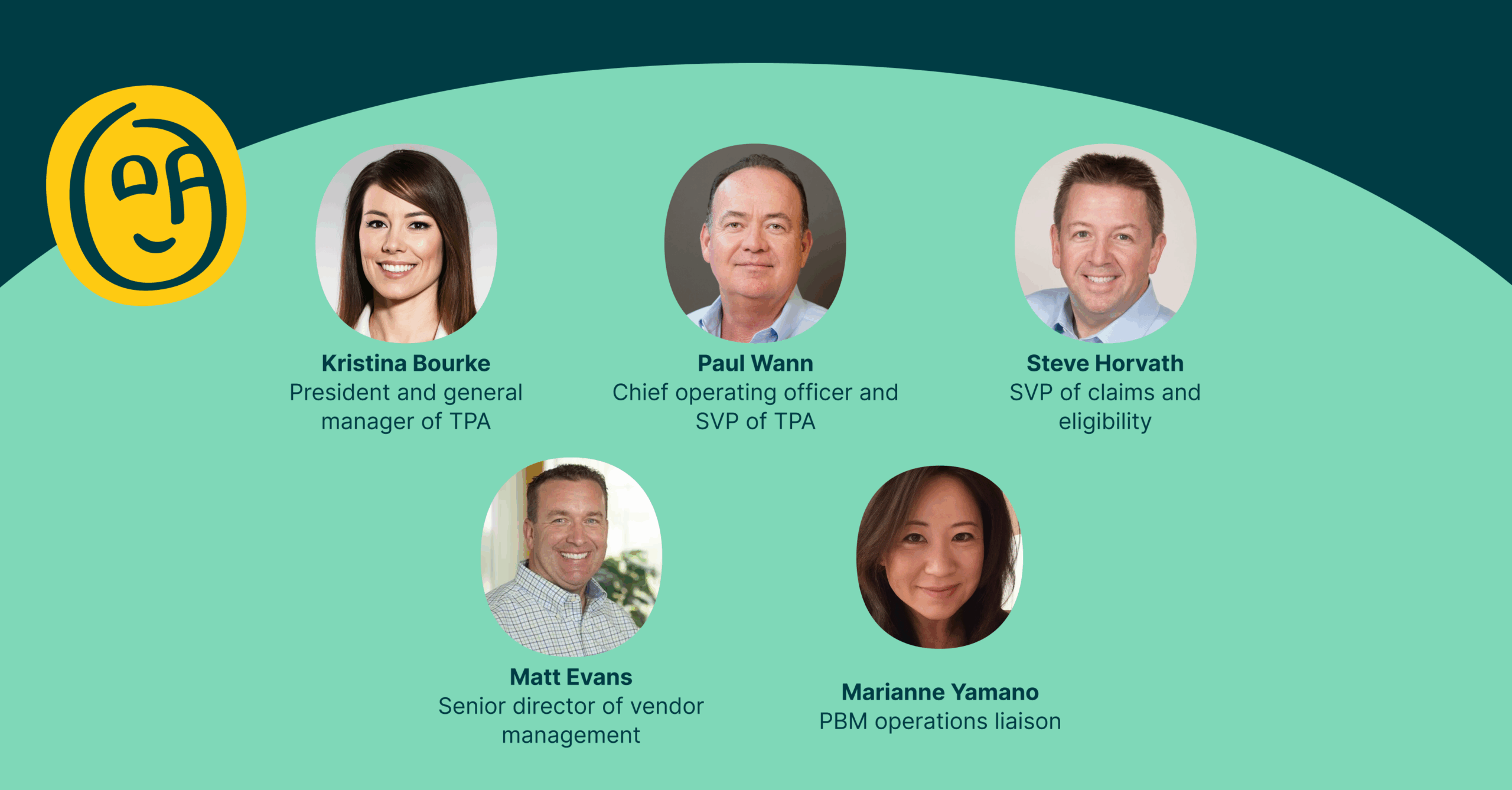
- Kristina Bourke, president and general manager of TPA, brings over 25 years of transformative leadership in healthcare services, including roles at Cloudmed, Vizient, and GE Healthcare IT. Her mastery of technology-enabled services with AI and strategic operations sets the stage for elevating Personify Health’s market presence while enhancing client engagement and satisfaction.
- Paul Wann, chief operating officer and SVP of TPA, adds more than three decades of deep knowledge in claims operations and software innovation from leading organizations such as Health Plans, Inc., Centivo, and Consociate Health. Paul’s hands-on experience is driving operational excellence and seamless service delivery.
- Steve Horvath, SVP of claims and eligibility, leads both Claims Operations and Eligibility & Enrollment with a 35-year track record of applying healthcare expertise and business transformation to amplify digital innovation and operational efficiency. He held leadership roles at Trustmark, CoreSource, and Health Contact Partners.
- Matt Evans, senior director of vendor management, contributes 15+ years of multifaceted experience spanning payer, provider, PBM, TPA, and BPO sectors. Matt’s leadership in vendor selection, contract negotiation, and performance optimization strengthens our external partnerships and supports sustained growth.
- Marianne Yamano, PBM operations liaison, brings over a decade’s expertise in pharmacy benefit implementations and operations across market segments including Commercial, Medicare, and Medicaid. Her role ensures cohesive alignment of PBM operations with the broader team.
“I’m excited to join Personify Health at such a pivotal moment in its growth,” commented Paul Wann. “This is an organization deeply committed to transforming healthcare through technology, personalized care, and operational excellence. I look forward to working alongside this talented team to deliver exceptional service to our TPA clients, partners, and members. Together, we’ll continue to push boundaries, optimize performance, and make a meaningful impact on the lives of those we serve.”
Investing in World-Class Member Services
To continuously raise the bar on member experience, Personify Health has invested significantly in state-of-the-art tools and dedicated teams:
- AI-powered learning platforms empower our service teams with real-time insights and upskilling opportunities, enhancing their ability to deliver empathetic, efficient support.
- Our dedicated service recovery team, launching this fall, will provide comprehensive end-to-end case resolution, driving faster, more compassionate outcomes while identifying root causes to prevent recurring issues.
Investments like these, alongside a team committed to continuous improvement, have driven outstanding member experience metrics:
- Customer Satisfaction (CSAT) increased 15% year-over-year, reaching an impressive 92%.
- Average Speed of Answer (ASA) accelerated to under 25 seconds – 44% faster than previous periods.
- First Call Resolution (FCR) consistently exceeds 90%, minimizing repeat contacts.
- Call Abandonment Rate is now below 5%, reflecting improved accessibility.
Advancing Claims Operations with Precision and Innovation
Personify has also made strategic enhancements in claims operations that reinforce our commitment to speed, accuracy, and quality:
- Increased Claims Operations staff by 19% in Q2 to meet growing demands.
- Total claim inventories declined by 14% in the last 30 days due to aggressive workflow improvements.
- Deployment of automation tools reduces manual processing, accelerates throughput, and boosts accuracy.
- New audit functionalities strengthen claim quality reviews, ensuring compliance and minimizing errors.
Looking Ahead
Personify Health’s strengthened leadership and targeted investments are elevating current performance while laying a strong foundation for future innovation and growth. Together, we are empowering our clients and members with smarter, faster, and more impactful healthcare administration services.
If you’re ready to challenge the old TPA model and put people at the center, let’s talk. Contact us, and let’s build something better – together.



